The Demand for Digital Pathology
When it comes to cancer, patients’ greatest fear is diagnostic delays—and they believe digital pathology and AI can reduce those delays
What health event are you most afraid of? For many, the answer is a cancer diagnosis—a piece of life-changing news that carries with it a host of additional worries. What’s more, a recent survey by Public First and the University of Cambridge has revealed that people’s greatest fear with respect to cancer is that the disease will be detected too late for effective treatment.1 Over two-thirds of respondents listed that as their primary concern—ahead of pain, treatment side effects, or the impact on family and friends.
One reason cancer instills so much anxiety is that almost everyone has firsthand experience with the disease—whether it’s a personal encounter or that of a loved one. “Everyone has a horror story associated with it,” says Nathan Buchbinder, cofounder and chief strategy officer at Proscia. “It becomes a cycle of fear. But why do we continue to feel that fear? I think it’s because of the unknowns.”
Buchbinder points out that no two people have the same experience, even if they are diagnosed with the same cancer. This uncertainty includes the possibility of pain, side effects, recurrences or metastases, severe illness, and even death—all of which are more likely the longer the disease goes undetected.
Diagnosing delays

It’s no surprise that many people fear a delayed diagnosis of cancer when the first obstacles arise before the process even begins. Many cancers present with nonspecific symptoms like fatigue, fevers, or weight loss, so patients and healthcare providers may not realize something is amiss. Once they do, geographic, financial, and psychological barriers may stand in the way of accessing necessary healthcare.
“In the laboratory itself, I think clinical lab professionals face a fundamental challenge: the demand for pathology services is far outpacing the number of skilled lab professionals available to handle it,” says Buchbinder. The numbers bear this out—in the UK, where the original survey was conducted, the Royal College of Pathologists found that only 3 percent of labs were adequately staffed to meet clinical demand.2 With workloads high and rising, the potential for diagnostic error cannot be overlooked.3
Other challenges add to the burden. “Inefficient workflows, insufficient access to experts, and inherent variability in test interpretation can all delay the care patients desperately need to avoid disease progression,” Buchbinder explains. “There can be only one consequence of this, and it’s not better outcomes.”
A technological paradigm shift
In January 2024, the Institute of Biomedical Science issued six key recommendations for reducing cancer testing delays: grow the workforce, bring cancer testing together, enable providers to deliver, improve data, develop an accountability framework, and invest in the fundamentals.4 The ideas are good in principle—but making them a reality is another story.
“If there were an easy solution, labs would be implementing it,” says Buchbinder. “The best approach will come from a paradigm shift in our approach to diagnostic medicine. And if it can’t come from staffing, it will have to come from technology.”
That’s why Buchbinder is an avid proponent of digital and computational solutions for the lab.
“There are many ways in which digitization drives efficiency, quality improvements, optimized resource utilization, and new insight through artificial intelligence (AI) solutions that change the way patients get diagnosed,” he says.
His list of potential gains includes:
- Remote consultation: “You’re no longer bound by the silos that have encapsulated the laboratory system in the past. You can access experts not only within your network, but even more broadly.”
- Economies of scale: “Labs can operate digitally as a single unified lab rather than being tied to the physical location where the staining, cutting, and fixing are done,” he says—which allows labs to exchange cases and share subspecialist expertise.
- Efficiency gains: “I think the biggest return on investment comes when you apply AI within that lab ecosystem. You enable workflow automation that can eliminate redundancies and take over the repetitive or time-consuming aspects of lab work.”
- Enhanced diagnosis: “AI can have a huge impact on decisions about when to treat, what treatments to use, and what the care team should be doing beyond the initial assessment. It changes the equation dramatically and may ultimately lead to further investment in the laboratory.”
This last item is where Buchbinder envisages the greatest gains—not just for patients, but for lab professionals as well. “I think we’ll see a shift in the economics of laboratory medicine and patient care, with additional investment going toward getting the most accurate and precise diagnosis possible. Ultimately, it leads to less expensive, higher-quality outcomes for patients.”
The demand is out there
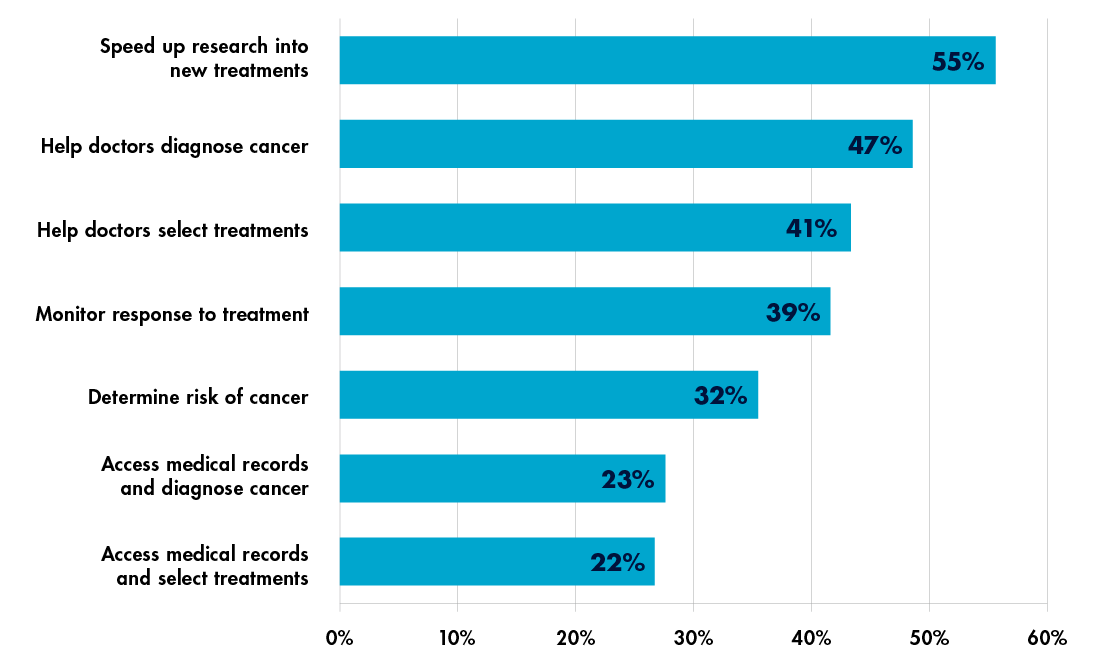
Although digital and AI-based tools can lower pathologists’ workloads, increase their comfort, and potentially alleviate pressure and burnout,5 it’s not only laboratorians who want a digital future—patients’ desire for these technologies is clear. Over half of respondents in the Public First survey wanted to see cancer diagnosed and treated earlier; a similar number reported that having tools to enable early detection would make them less afraid of a future cancer diagnosis. Enthusiasm for AI was evident in a range of applications from basic research to diagnosis and treatment selection (see Figure 1).
In these responses, Buchbinder sees a new pressure arising for laboratories—one he believes will reshape laboratory medicine as much as the imbalance between supply and demand. As the use of precision medicine increases,6 he foresees that labs will be challenged with delivering an altogether new type of service.
“We’re seeing more and more treatments come out that are tied to specific biomarkers or companion diagnostics,” he says. “Those treatments are more targeted. They’re more cost-effective. They work better for patients. That is the way of the future—and laboratories play an essential role.”
Buchbinder’s concern, though, is that today’s specialty testing is a complicated process that often necessitates outsourcing. His vision is different.
“I think the AI companion diagnostic technology coming into play today will allow labs to perform complex precision diagnostics themselves.7 In this landscape, the lab becomes the provider of not just a diagnosis, but also deep insight and guidance that informs what the rest of the care team does. That means increased interaction between the lab and other subspecialties. It means re-equipping the lab to be technology-first. And it means rethinking the financial and operational aspects of laboratory medicine as a whole. That’s what I see when I picture the lab of the future.”
References:
- Brierley C. Cancer is the public’s biggest health concern. University of Cambridge. July 15, 2024. https://www.cam.ac.uk/stories/2024-cancer-polling.
- Royal College of Pathologists. Meeting pathology demand: Histopathology workforce census. August 2018. https://www.rcpath.org/static/952a934d-2ec3-48c9-a8e6e00fcdca700f/Meeting-Pathology-Demand-Histopathology-Workforce-Census-2018.pdf
- Khatab Z et al. Pathologist workload, burnout, and wellness: connecting the dots. Crit Rev Clin Lab Sci. 2024;61(4):254–274. doi:10.1080/10408363.2023.2285284.
- Institute of Biomedical Science. Time to Test – creating the capacity the NHS needs for the future of cancer testing. January 24, 2024. https://www.ibms.org/resources/documents/time-to-test-creating-the-capacity-the-nhs-needs-for-the-future.
- Williams B. The value of digital pathology. Digital Pathology Association. January 18, 2018. https://digitalpathologyassociation.org/blog/the-value-of-digital-pathology.
- Muharremi G et al. The buzz surrounding precision medicine: the imperative of incorporating it into evidence-based medical practice. J Pers Med. 2023;14(1):53. doi:10.3390/jpm14010053.
- Johnson KB et al. Precision medicine, AI, and the future of personalized health care. Clin Transl Sci. 2021;14(1):86–93. doi:10.1111/cts.12884.
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article