Could CRISPR-Based Options Be the Next Generation of COVID-19 Diagnostics?
While it may be in retreat, COVID-19 is unlikely to perish completely from the earth. And even if it does, some other nefarious form of infectious agent is bound to emerge. All of this creates an urgent need for simple, scalable, and rapid diagnostics capable of detecting the SARS-CoV-2 virus at the point of care. While they may suffice for the moment, molecular, antigen, and antibody tests in current use have significant limitations. However, researchers and laboratory companies are hard at work developing alternatives. Perhaps the most promising of these is testing based on clustered regularly interspaced short palindromic repeats (CRISPR) to detect genetic material associated with the virus. The Diagnostic Challenge Of course, molecular detection of SARS-CoV-2 DNA is also the basis of current tests. Coronaviruses are single-stranded RNA (ssRNA) viruses with eight accessory proteins and four major structural proteins. Current tests target different components to detect SARS-CoV-2, including the spike protein (S), small envelope protein (E), nucleocapsid protein (N), and RNA-dependent RNA polymerase (RdRp) gene of the ORF1ab sequence. The most commonly used method of COVID-19 detection, reverse transcription quantitative polymerase chain reaction (RT PCR), is considered to be the gold standard for accuracy. However, RT PCR is […]
The Diagnostic Challenge
Of course, molecular detection of SARS-CoV-2 DNA is also the basis of current tests. Coronaviruses are single-stranded RNA (ssRNA) viruses with eight accessory proteins and four major structural proteins. Current tests target different components to detect SARS-CoV-2, including the spike protein (S), small envelope protein (E), nucleocapsid protein (N), and RNA-dependent RNA polymerase (RdRp) gene of the ORF1ab sequence. The most commonly used method of COVID-19 detection, reverse transcription quantitative polymerase chain reaction (RT PCR), is considered to be the gold standard for accuracy. However, RT PCR is not totally free of accuracy issues and has been shown as being apt to produce false negative results. More significantly, given current needs, it is also slow and capital-intensive to the extent it relies on the use of sophisticated equipment and trained laboratory scientists to convert RNA from the sample to DNA, which then must be amplified to generate millions of copies for testing. Tests detecting antibodies the body forms to fight the virus or the antigens produced by those antibodies are faster, simpler, and less expensive, making them ideal for use at the point of care. However, they lack the sensitivity and specificity of RT PCR tests. Recently, the U.S. Food and Drug Administration (FDA) has had to recall widely used at-home antigen kits due to the potential for false positives.The Promise of CRISPR Testing
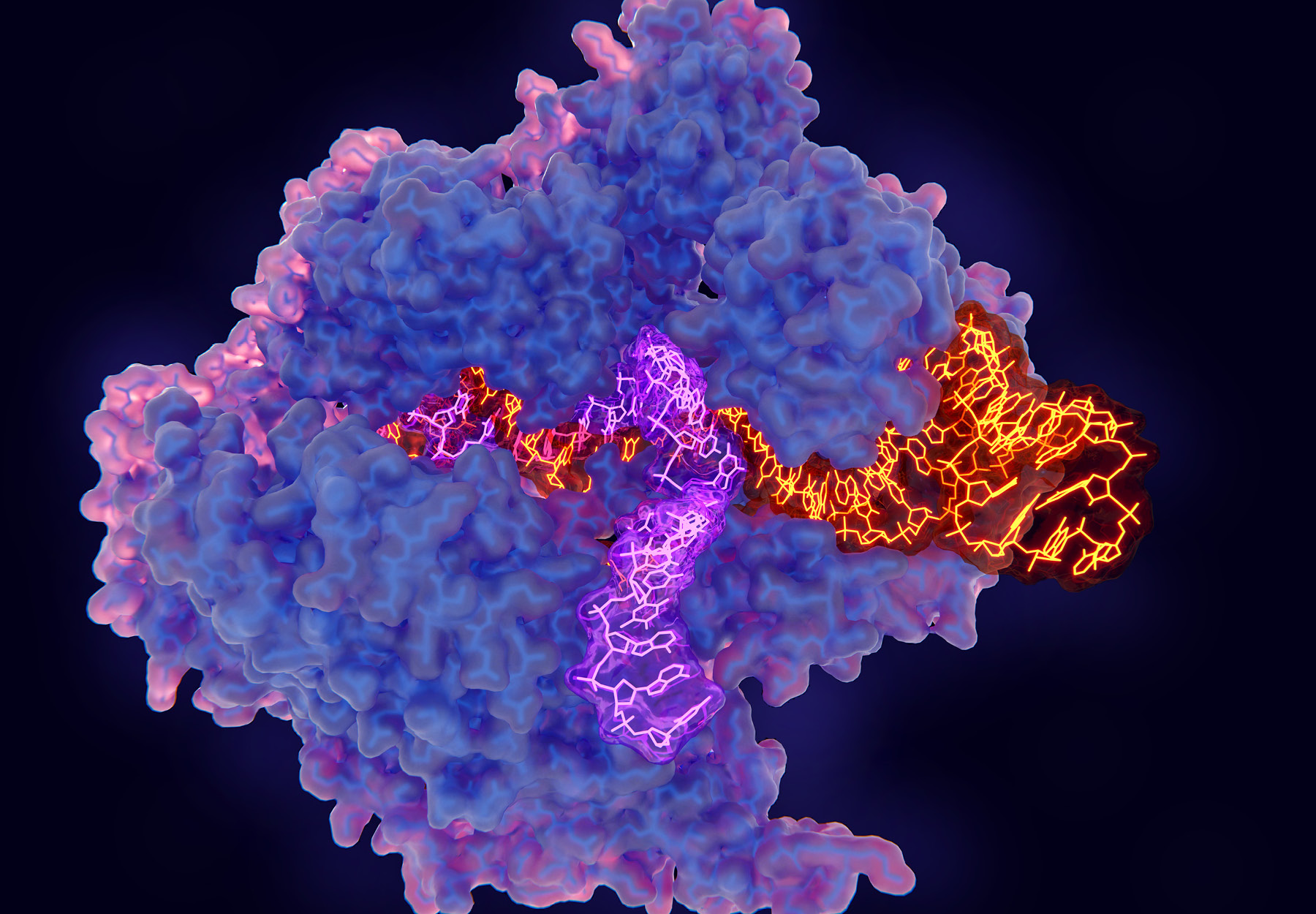
CRISPR/Cas-based nucleic acid detection offers simplicity, speed, high sensitivity, and specificity. The CRISPR RNA cuts the target region. CRISPR Cas12, Cas13, and Cas14 proteins can then bind to a complementary DNA sequence, which is subsequently cleaved via Cas endonuclease activity:- Cas12 recognizes double-stranded DNA (dsDNA) more efficiently than ssDNA, but still exhibits collateral activity for ssDNA;
- Cas14 recognizes ssDNA more effectively than dsDNA with respect to cleavage activity and also exhibits collateral activity for ssDNA;
- Cas13 is unique because it recognizes and exhibits collateral activity for ssRNA.
The Race to Bring a CRISPR Test to Market
There are two notable efforts to bring a CRISPR-based rapid, point-of-care SARS-CoV-2 diagnostic to the US market. The first is spearheaded by a group of scientists from the University of California, Berkeley, led by biochemist Jennifer Doudna. A study by the Doudna team published in Nature Chemical Biology on August 5, 2021, supports the viability of a point-of-care diagnostic delivering reliable results from swab testing within 20 minutes. A month after the study, Mammoth Biosciences, the San Francisco-based biotech company that Doudna and her colleagues founded in 2017, raised $195 million in Series C and D financing rounds to develop and commercialize the test. The project also received federal funding through the National Institutes of Health’s Rapid Acceleration of Diagnostics Initiative, as well as the Department of Health and Human Services. Mammoth had another trump card: scientific instruments pioneer Agilent Technologies. For a year, the companies collaborated to develop the CRISPR test. The strategy: Tailor Mammoth’s CRISPR enzymes for identifying genetic codes to react with and identify the SARS-CoV-2 virus genome while Agilent leveraged its Bravo BenchCel DB workstation platform to deliver high-speed liquid handling hardware. The end result was the DETECTR Boost SARS-CoV-2 Reagent Kit assay, a high throughput platform capable of processing more than 4,000 tests per day. The DETECTR test performs simultaneous reverse transcription and isothermal amplification using loop-mediated amplification (RT-LAMP) for RNA extracted from oral or nasal swabs, with a total run time of 15 minutes. On Jan. 24, the US Food and Drug Administration (FDA) announced that it had granted Emergency Use Authorization (EUA) for the DETECTR test, the first high-throughput CRISPR-based SARS-CoV-2 assay to win such clearance. Mammoth and Agilent will launch the test under a comarketing agreement signed last January “This partnership will help address the need for more widespread testing options for COVID-19, helping to fill the gap in the market as testing labs run into supply issues or reach capacity,” noted Mammoth CEO Trevor Martin in a statement issued when the comarketing deal with Agilent was announced.The miSHERLOCK CRISPR-Based Saliva Device
Although Mammoth has won the race to bring a CRISPR test to market, a rival project is also nearing the finish line. Researchers at the Wyss Institute for Biologically Inspired Engineering at Harvard University and the Massachusetts Institute of Technology (MIT) have created a low-cost CRISPR-based diagnostic capable of detecting SARS-CoV-2 from saliva. Described in the August 6, 2021 issue of Science Advances, miSHERLOCK (mi stands for “minimally instrumented”) is based on the CRISPR platform developed by Sherlock Biosciences, a company co-founded by one of the researchers. The assay uses Cas12a guide RNA to distinguish different variants with a limit of detection of one molecule per microliter in unprocessed saliva, comparable to a RT PCR test. In experiments, the device successfully distinguished among three different SARS-CoV-2 variants and can be reconfigured to detect additional variants. The device can be assembled using a 3D printer and commonly available components for about $15. Re-using the hardware brings the cost of individual assays down to $6 each. “miSHERLOCK eliminates the need to transport patient samples to a centralized testing location and greatly simplifies the sample preparation steps, giving patients and doctors a faster, more accurate picture of individual and community health, which is critical during an evolving pandemic,” said co-first author Helena de Puig, PhD, a postdoctoral fellow at the Wyss Institute and MIT, in a Wyss article.Takeaway
The CRISPR-based assays provide PCR-equivalent performance but on a much more scalable and rapid basis, making them ideal for use in screening asymptomatic populations. With one product already on the US market and another close behind, CRISPR testing might very well represent the next generation of COVID-19 diagnostics.Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article