Early last month, the American Society for Gastrointestinal Endoscopy (ASGE) released a new guideline document on screening patients with genetic susceptibility for pancreatic cancer. Previous guidelines suggested that screening should be limited only to those with a family history of pancreatic cancer, whereas these new guidelines suggest that anyone with the BRCA1/2 pathogenic variant should be screened, regardless of their family history of the disease. The recommendations are not meant to be set rules or legal standards, but evidence-based suggestions for screening for these individuals, the ASGE states.
Based on evidence presented to a panel of experts and various stakeholders in gastroenterology, epidemiology, genetics, radiology, and oncology, as well as two patient advocates, the new guideline makes five key recommendations, noting that they are “conditional” as the evidence to support them was low or very low quality:
- Those with an increased risk of pancreatic cancer due to genetic susceptibility should be screened.
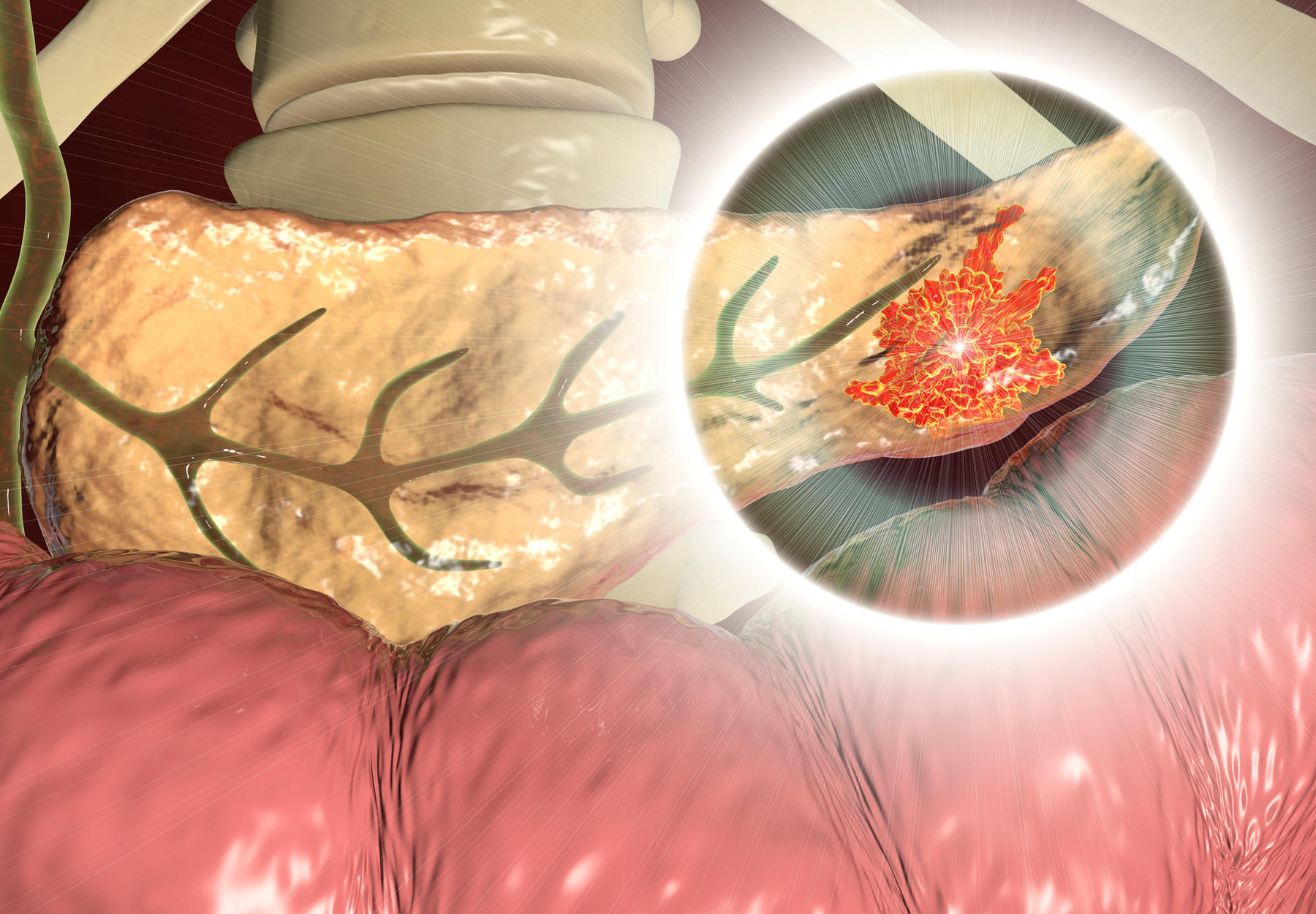
- In people with genetic susceptibility, it’s suggested that patients be screened with endoscopic ultrasound (EUS), EUS alternating with magnetic resonance imaging (MRI), or MRI, based on their preference and expertise available in their area.
- Suggest screening for those with the BRCA2 pathogenic variant.
- Suggest that those with genetic susceptibility should be screened for pancreatic cancer on an annual basis.
- Suggest that, in such individuals with genetic susceptibility, the starting age for pancreatic cancer screening should vary depending on the person’s underlining genetic condition
Given that pancreatic cancers made up three percent of all newly diagnosed cancer cases and eight percent of the total number of cancer-related deaths in the US in 2020, and that catching pancreatic cancer early is essential to increased survival rates, the guidelines aim to help clinicians reach diagnoses sooner, potentially prolonging many lives, the ASGE says.