Plugging Current Gaps in Cancer Screening Will Save Lives
COVID-19 is the curse that just keeps on giving. Countless numbers of people have put off cancer screenings as a result of the pandemic, and that may lead to a significant increase in cancer-related deaths in the coming years. That is the sobering conclusion of a new report released by the President’s Cancer Panel on Feb. 3. Cancer Screening Underutilization Improvements in early detection and treatment, coupled with reductions in smoking, have prevented an estimated 3.2 million cancer deaths in the US since 1991, according to the report from the panel, which was established in 1971 to monitor the progress of the National Cancer Program (NCP). However, too many people are still dying, with over 600,000 cancer deaths expected in 2021. In addition to the human toll, cancer deaths cost the US over $90 billion per year in lost earnings. One reason that cancer remains a major problem is that screening has been underutilized, both before and during the pandemic. Focusing on the four cancers—breast, cervical, colorectal, and lung—for which the U.S. Preventive Services Task Force (USPSTF) recommends screening for eligible individuals, the report describes “significant gaps between recommended screening and screening uptake.” Source: President’s Cancer Panel, “Closing Gaps in […]

Cancer Screening Underutilization
Improvements in early detection and treatment, coupled with reductions in smoking, have prevented an estimated 3.2 million cancer deaths in the US since 1991, according to the report from the panel, which was established in 1971 to monitor the progress of the National Cancer Program (NCP). However, too many people are still dying, with over 600,000 cancer deaths expected in 2021. In addition to the human toll, cancer deaths cost the US over $90 billion per year in lost earnings. One reason that cancer remains a major problem is that screening has been underutilized, both before and during the pandemic. Focusing on the four cancers—breast, cervical, colorectal, and lung—for which the U.S. Preventive Services Task Force (USPSTF) recommends screening for eligible individuals, the report describes “significant gaps between recommended screening and screening uptake.”Source: President’s Cancer Panel, “Closing Gaps in Cancer Screening.” The report notes that the table may not be comprehensive.
Rates are particularly low for lung cancer, partly because screening has only been recommended since 2013. Colorectal cancer screening has increased in recent years, but gaps remain. While screening rates for breast and cervical cancer have risen, they have plateaued in the past 20 years. In addition, the report notes, many people at high risk for cancer due to their personal or family history are not being identified or offered appropriate high-risk screening.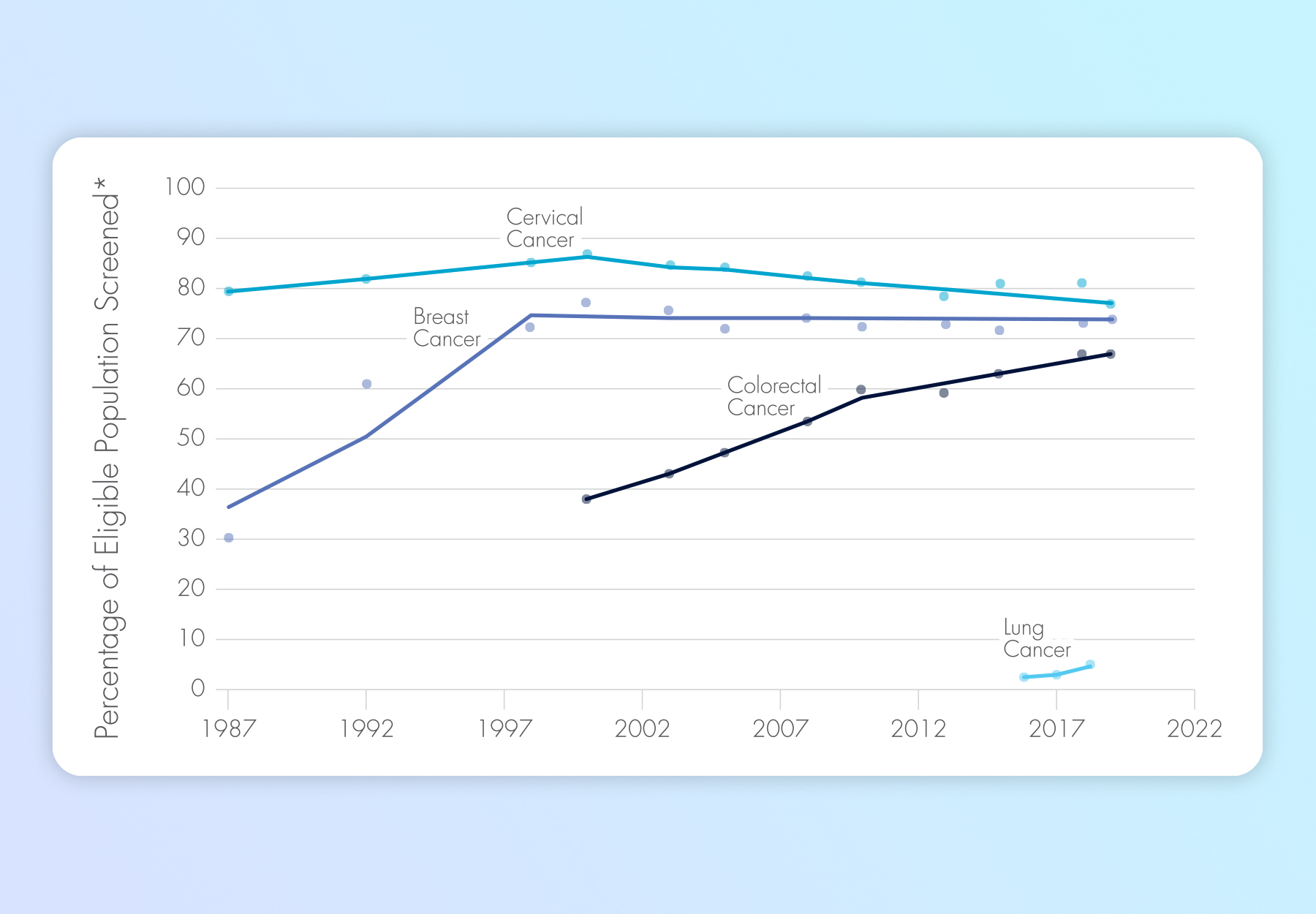
Source: President’s Cancer Panel, “Closing Gaps in Cancer Screening.” The report notes that the table may not be comprehensive. *More specifics can be found in the report.
Cancer Screening During the Pandemic
Not surprisingly, the COVID-19 pandemic has exacerbated the problems. Cancer screening plummeted in the spring of 2020 when many health care services had to be suspended and people were ordered to stay at home. Many within the cancer community expressed concerns that delayed and missed diagnoses would result in nearly 10,000 excess breast and colorectal cancers in the US over the next 10 years. While screening has resumed, the report notes that rates continue to fluctuate and remain below pre-pandemic rates. The report says that the pandemic provides four lessons about cancer screening:- Cancer screening is an essential health care service and should not be delayed or forgone except when the risks clearly outweigh benefits;
- Clear and accurate communication is necessary to guide screening during health care system disruptions;
- High-risk individuals should be identified and prioritized when screening capacity is limited; and
- Telehealth and self-collection may enable screening for certain cancers with minimal physical contact with health care settings.
The Panel’s 4 Recommendations
The Bottom Line: Cancers are not being detected and treated early and people are unnecessarily dying or enduring aggressive treatment that screening could have prevented. The report notes that this has a disproportionate impact on people of color and other socially and economically disadvantaged populations, as well as those at genetically elevated risk of cancer. For the panel, more robust screening is the key to resolving the cancer problem. The report says that the NCP has a “significant opportunity” to “accelerate the decline in cancer deaths” and further early cancer detection and removal of precancerous lesions by promoting more effective and equitable implementation of cancer screening. The panel sets out four broad sets of goals for the NCP to pursue to close the current screening gaps:-
Improve and Align Cancer Screening Communication
- Conduct large- and small-scale communications campaigns; and
- Create and expand National Cancer Roundtables to address screening gaps.
-
Promote Equitable Access to Cancer Screening
- Provide and sustainably fund community-oriented outreach and support services to promote appropriate screening and follow-up care; and
- Increase access to self-sampling for cancer screening.
-
Bolster Collaborations between Cancer Screening and Cancer Risk Assessment
- Empower health care team members to support screening, such as by expanding Medicare and Medicaid coverage requirements so that a wider array of providers can support cancer screening for their patients; and
- Expand access to genetic testing and counseling for cancer risk assessment.
-
Create Health Information Technology that Promotes Cancer Screening
- Create computable versions of cancer screening and risk assessment guidelines; and
- Create and deploy effective CDS tools for cancer risk assessment and screening.
Presidential Cancer Panel Calls on Payors to Loosen the Reins on Genetic Testing
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article