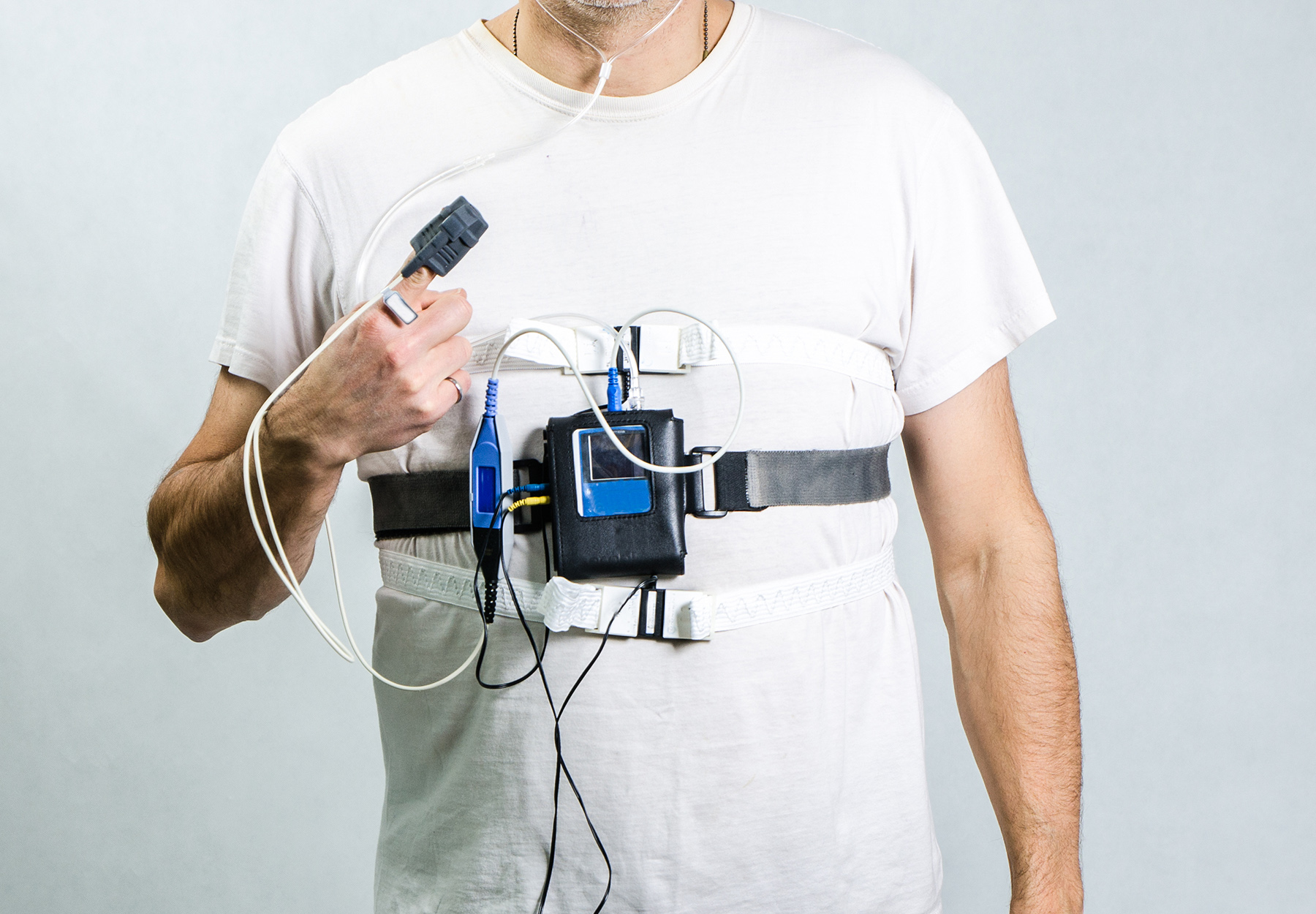
False billing of home sleep tests to diagnose obstructive sleep apnea (OSA) has been on the radar of federal fraud enforcers and whistleblowers for nearly a decade. The most recent case began when whistleblowers filed a qui tam lawsuit against Chicago area-based national sleep lab SNAP Diagnostics and two of its officers. They claimed that the officers directed SNAP to submit claims for Medicare patients’ second and third nights of home sleep testing knowing that it needed only one night of testing to effectively diagnose OSA and that it routinely tested and claimed only one night for privately insured patients. In addition to defrauding five federal agencies, they accused SNAP of illegally multiplying the copays it received from Medicare beneficiaries.
And that’s not all. The whistleblowers claimed that SNAP paid kickbacks for home sleep testing referrals by:
- Offering to interpret certain sleep tests of commercially insured patients and then providing the referring physicians an unsigned report—essentially a blank check that physicians could sign and use to seek reimbursement for the professional component of the test;
- Using an independent contractor salesforce but paying it volume-based commissions; and
- Offering to waive the copays on sleep tests for providers and members of their family or staff.
SNAP vigorously denied the allegations. But when the federal government decided to intervene, the pressure to settle intensified. Under the settlement, SNAP will pay $3.925 million, with $300,000 coming from the company’s founder and $125,000 from its vice president. SNAP also has to enter into a corporate integrity agreement requiring the firm to hire an independent organization to perform an annual review of claims and submit reports to the Office of Inspector General for the U.S. Department of Health and Human Services.