The Latest Developments in Liquid Biopsy and ctDNA Testing
The latest developments in liquid biopsy and ctDNA testing and why they should be of interest to clinical laboratory professionals
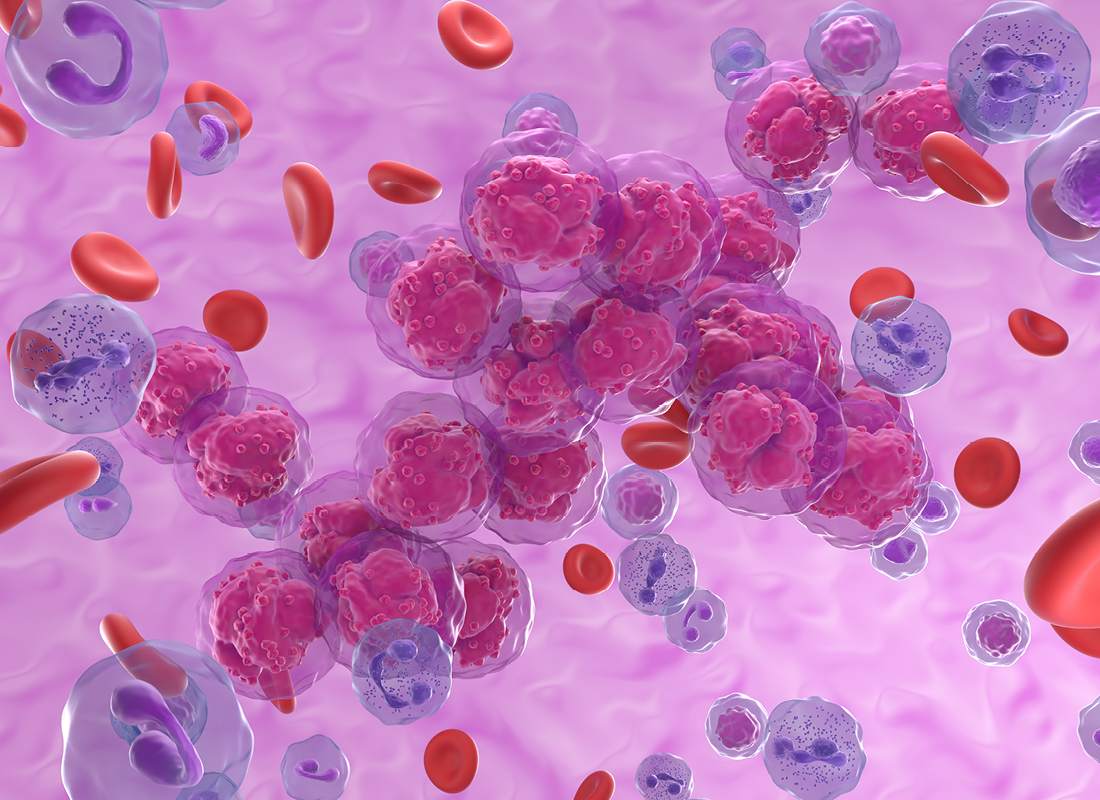
Liquid biopsy and circulating tumor DNA (ctDNA) testing have seen rapid growth over the past decade—not only offering a simpler, less invasive, and more powerful tool for cancer diagnosis and monitoring, but also opening the door to new modalities for precision oncology testing, profiling, and treatment.1
In this dynamic landscape, staying abreast of liquid biopsy developments and applications is key for clinical laboratory professionals given the widespread and growing attention these diagnostics are garnering.2 So, what recent progress has been made in liquid biopsy and ctDNA testing—and what is the future for these technologies in the clinical lab?
Fleeting traces of ctDNA complicate liquid biopsy
Since the first identification of circulating tumor cells in 1869,3 tools capable of precisely analyzing fluid specimens to detect—and even predict—the presence of cancers in their earliest stages have made substantial progress. This has come not only in the widened scope of components identifiable within the tumor circulome,4 but also in new methods of collection, processing, and assessment.
Despite this, the technologies’ true potential has yet to be realized. This is in part caused by the low abundance of ctDNA, especially for small tumors, which creates difficulty in collecting sufficient blood for adequate detection and in accurately distinguishing between ctDNA—consistently eliminated from circulation in as little as 30 minutes—and other cell-free DNA.
To surmount the challenge insensitivity poses, laboratorians frequently rely on ex vivo sequencing and amplification. However a Massachusetts-based research team recently reported two novel priming agents that, when given one to two hours before drawing blood, temporarily but substantially elevated serum ctDNA levels.5 One of the agents consists of lipid-covered nanoparticles that inhibits ctDNA uptake by Kupffer cells in the liver; the other is an antibody that binds ctDNA and shields it from DNases. Both were shown to attenuate ctDNA clearance in vivo, resulting in the transient augmentation of ctDNA. This enabled over 10-fold ctDNA recovery and more complete tumor molecular profiling, as well as improved detection sensitivity—which, in the case of small tumors, increased from less than 10 percent to more than 70 percent.
“This study is very exciting in that it addresses one of the major issues with liquid biopsies,” Maria Arcila, MD, director of the Diagnostic Molecular Pathology Laboratory at Memorial Sloan Kettering Cancer Center, told the National Cancer Institute.6
“This is very early data,” said Arcila, who was not involved in the study. However, she added that the priming agents’ potential to improve liquid biopsies’ cancer-detecting ability “is very encouraging.”6
These preliminary experiments were conducted in a mouse model and therefore still need to be not only verified in humans, but also proven safe—especially given that there are likely biological reasons for the rapid clearance of serum ctDNA. Some of the researchers involved in the work have formed a company to progress both approaches, including into human testing, so these early results may form the basis of eventual advances that expand liquid biopsy’s diagnostic potential.
Prediction power with ctDNA testing
Advances in ctDNA amplification aren’t the only exciting developments in this domain.
“I think the future is very bright,” says Isaac Garcia-Murillas, staff scientist in the Molecular Oncology Group at London’s Institute of Cancer Research, who has focused on identifying ctDNA biomarkers with clinical utility since 2013. “CtDNA analysis is now a reality in advanced settings in some solid tumors and is starting to be offered routinely. As we deploy these assays in more patients and use the results to guide clinical interventions, their clinical utility will be cemented. In the early setting, we’re still lagging a bit behind, but it’s coming.”
Garcia-Murillas and his team showcased a glimpse of this bright future and the true predictive potential of these technologies at this year’s American Society of Clinical Oncology annual meeting.7 There, they presented results of a forthcoming study in which they predicted breast cancer recurrence in high-risk patients up to 3.5 years before relapse.
“This is a proof-of principle retrospective study on early breast cancer patients using a novel approach based on whole genome sequencing rather than the current whole exome sequencing approaches,” Garcia-Murillas explains. Using genomic sequencing increased the scope of cancer-related changes the researchers could identify within a patient’s DNA, combating the insensitivity issue.
“By tracking a larger number of mutations—up to 1,800 in this case—we show that sensitivity can be improved, thus allowing earlier detection of ctDNA,” he says, “We were able to identify ctDNA in all of the women who subsequently clinically relapsed, whereas none of the women who had no ctDNA detected during follow-up relapsed during the study.”
As with the in vivo amplification study, these promising results are just the first step in a long journey, but one that could eventually lead to the routine clinical use of highly accurate predictive ctDNA tests.
“The work we have presented is the first stage,” explains Garcia-Murillas. “We now need to deploy this approach in prospective interventional trials to ascertain its clinical validity. This should be done under a phase III trial within a large population. Although some tests that detect minimal residual disease are already being tested in this way—and some are, for example, Medicare approved—I believe we are still a few years away from the clinical utility of ctDNA in the early setting.”
Wait and see stance for clinical labs
What exactly do these developments mean for laboratorians’ day-to-day work? Because they’re in the early stage, little to nothing will change immediately. Even when such advances do eventually make it to the clinical lab, Garcia-Murillas doesn’t believe they’ll necessarily upend the status quo.
“I don’t think it will change much for those professionals already running next-generation sequencing approaches in ctDNA in either the early or the advanced setting,” he says. “It is another assay, although it will require different validated wet-lab workflows and more complex bioinformatics pipelines for analysis.”
But there are still things he believes the clinical laboratory should do to stay at the forefront of ctDNA and liquid biopsy testing, both now and as future developments arise. He recommends labs should:
- Be well versed in preanalytical workflows to have the best-quality samples going into analysis
- Have expertise in next-generation sequencing workflows from the wet lab to bioinformatic analysis and data interpretation
- Possess a clear idea of how to report complex results to medical colleagues and help with related interpretation
- Employ robust data storage and access policies
Clinical lab leaders may also want to explore how artificial intelligence can influence ctDNA testing, particularly the predictive aspects of it. In a May 2024 article, Today’s Clinical Lab—a sibling publication of Clinical Diagnostics Insider—outlined the benefits of applying artificial intelligence to advance noninvasive cancer screening.
References:
- Lone SN et al. Liquid biopsy: a step closer to transform diagnosis prognosis and future of cancer treatments. Mol Cancer. 2022;21(1):79. doi:10.1186/s12943-022-01543-7.
- Batool SM et al. The liquid biopsy consortium: challenges and opportunities for early cancer detection and monitoring. Cell Rep Med. 2023;4(10):101198. doi:10.1016/j.xcrm.2023.101198.
- Ashworth TR. A case of cancer in which cells similar to those in the tumours were seen in the blood after death. Aust Med J. 1869;14(1):146–149.
- Alba-Bernal A et al. Challenges and achievements of liquid biopsy technologies employed in early breast cancer. EBioMedicine. 2020;62(1):103100. doi:10.1016/j.ebiom.2020.103100.
- Martin-Alonso C et al. Priming agents transiently reduce the clearance of cell-free DNA to improve liquid biopsies. Science. 2024;383(6680):eadf2341. doi:10.1126/science.adf2341.
- Philips C. Pump Up the Volume: “Priming Agents” May Improve Cancer Liquid Biopsies. February 22, 2024. https://www.cancer.gov/news-events/cancer-currents-blog/2024/liquid-biopsy-increase-ctdna-in-blood.
- The Institute of Cancer Research. ASCO 2024: New ultra-sensitive blood test predicts recurrence of breast cancer, months or even years before relapse. June 1, 2024. https://www.icr.ac.uk/news-archive/asco-2024-new-ultra-sensitive-blood-test-predicts-recurrence-of-breast-cancer-months-or-even-years-before-relapse.
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article