The Promise of State-of-the-Art Sequencing Technologies for Cancer Screening
Circulating tumor DNA sequencing technologies are tackling the challenges of early cancer detection.

Imagine a diagnostic technology that could detect cancer at the earliest stages before tell-tale symptoms arise. A platform that could not only track the warning signs for a wide array of cancer types, but could also chart the location from where the signals originate. Now envision that all this exquisite insight could be gleaned from a simple sample of blood.
This is not a far-off dream—this is reality. Breakthrough DNA sequencing technologies are making an unprecedented impact on the once sacred territory of cancer screening. Combining non-invasive patient sampling with state-of-the-art sequence analysis, these emerging solutions may signify a revolution in cancer early detection and disease prevention.
The Diagnostic Challenge
Early detection has historically been one of the major challenges for accurate diagnosis and treatment of cancer. Each cancer type presents with its own set of symptoms, which are subsequently confirmed by imaging, biopsy, and pathology analysis. High-resolution magnetic resonance imaging (MRI) or positron emission tomography (PET) scans can visualize the location and size of the tumor. Pathology examination of biopsied tissue can identify the cell morphology and biomarkers indicative of the tumor type and stage. Further tests can disclose the extent to which other sites are involved. Taken together, this information informs doctors whether the tumor is indeed malignant, the extent of its growth and damage to surrounding tissue, and the potential for progression based on the tumor type and stage.
Screening technologies exist for a growing number of common cancers. For instance, routine mammograms are now standard of care for breast cancer screening. Early-stage prostate cancer can be detected by screening for elevated levels of prostate specific antigen (PSA). Screening for colon cancer has benefited from colonoscopy, while cervical cancers are routinely screened by Pap and human papillomavirus (HPV) tests.
Many more cancer types can be genetically profiled through DNA sequence analysis, looking at underlying genetic signatures present in the patient’s DNA—either germline (inherited) or somatic (acquired). Knowing whether these signatures will evolve into cancer and if so, when and to what extent, can be a challenge.
Moreover, despite current approaches toward early detection, most cancers show no symptoms until later stages, when treatment options are limited and outcomes can turn deadly. Approximately 70 percent of cancer deaths are caused by cancers that are not commonly screened against1.
State-of-the-Art Screening Solutions
Recent leaps in technology have made it possible to sequence patient tumor DNA using minimally invasive techniques, providing clinically actionable data on the type, stage, and origin of the tumor itself. Several new technology platforms have combined these attributes with screening capabilities for multiple cancers, including many of those previously intractable to early detection.
A Non-Invasive Screen for Colon Cancer
Colon cancer is the third most common cancer in the US, with over 100,000 new cases estimated each year. Current American Cancer Society (ACS) recommendations2 include starting screening at age 45 using either a visual exam such as a colonoscopy, or a stool-based test. Colon cells routinely shed DNA, which can be isolated and analyzed for the presence of cancer signatures. Tests like Cologuard®3 have proven capable of detecting precancerous polyps and cancer cells from stool samples, with a 92 percent accuracy rate. Although not as comprehensive as a diagnostic colonoscopy, which can detect and locate precancerous colon lesions, tests like Cologuard® offer fast, minimally invasive results for use as a periodic screening solution. Developed and commercialized several years ago, the success of Cologuard® was proof-in-concept that non-invasive DNA analysis is a viable and effective cancer screening approach.
Liquid Biopsy and Circulating Tumor DNA
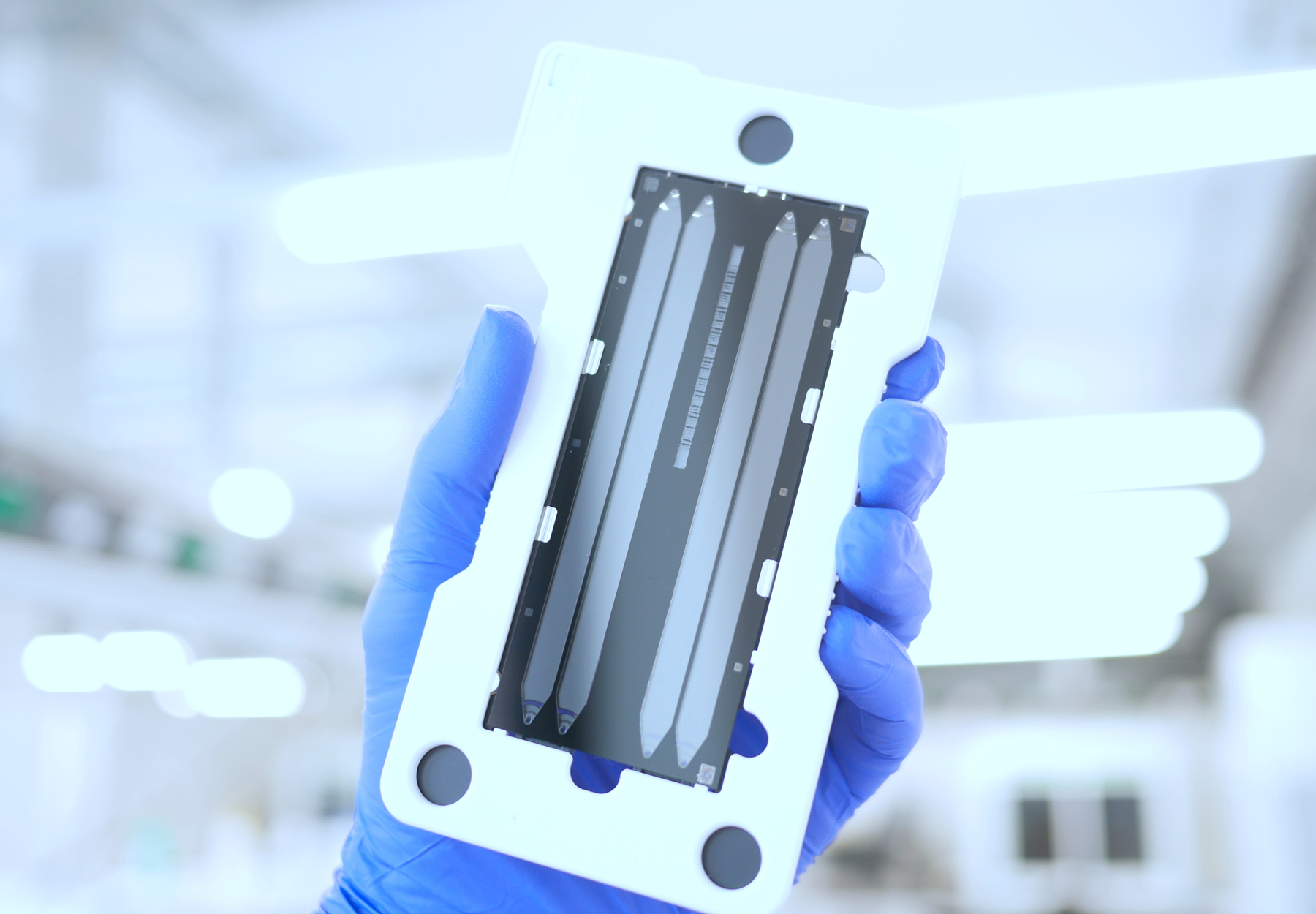
“Liquid biopsy” is a term that has gained significant notoriety in clinical and diagnostic circles. Unlike conventional sequencing techniques, which require primary patient tissue such as that taken during pathology biopsy, liquid biopsy involves analyzing a patient’s blood for the presence of protein or genetic markers of disease. As a minimally invasive platform, liquid biopsy analysis has proven useful for detection of several diseases, including various types of cancer, infectious diseases, and a growing list of others.
The detection of cancer from liquid biopsies depends on the availability of freely floating DNA fragments called cell-free DNA (cfDNA) or, more specifically, circulating tumor DNA (ctDNA) that are shed during tumor apoptosis or necrosis. Although the fragments are typically removed by macrophages, overproduction from cancer cells leaves more of the ctDNA behind, providing a robust, non-invasive marker of disease.
Thermo Fisher Oncomine Dx Target test
Thermo Fisher Scientific originally developed and commercialized the Oncomine Dx Target test4 as the first in vitro diagnostic for non-small cell lung cancer (NSCLC) and cholangiocarcinoma. Based on the Ion Torrent NGS technology and leveraging liquid biopsy analysis, the Oncomine test proved capable of detecting multiple biomarkers for a range of targeted therapies from a single sample with a four-day turnaround. The FDA recently approved5 the test as a companion diagnostic to aid in selection of patients with RET-fusion positive advanced or metastatic NSCLC and thyroid cancer who may be eligible for treatment with drugs such as Retevmo®6, a RET kinase inhibitor. This was the latest approval for the test, which had previously obtained companion diagnostic status for 15 other targeted therapies, helping to quickly match patients with the appropriate targeted therapeutic approach.
Foundation Medicine FoundationOne® CDx and Liquid CDx
Foundation Medicine has built a portfolio7 of companion diagnostics and FDA-approved comprehensive genomic profiling (CGP) tests that function across multiple cancers. CGP tests can inform early treatment options based on the unique genomic profile of a patient’s tumor. Foundation Medicine’s CGP tests are based on tissue or peripheral whole blood, analyzing over 300 genes for signatures including tumor mutational burden (TMB), microsatellite instability (MSI), and further genomic features.
As opposed to smaller marker panels and later-stage companion diagnostics, these CGP tests can produce comprehensive profiling information in a single test sample and provide information on the complex signature of an individual patient’s cancer. This information can then help in characterizing the tumor at an early stage and informing the best course of action, such as the use of targeted therapies, immunotherapies, tumor-agnostic treatments, and/or clinical trials.
Methylation-Based Analysis Using NGS Technologies
A major caveat of liquid biopsy analysis is the necessity for enough ctDNA to allow detection. Many tumors in the early process of proliferation fail to meet this obligation. The amounts of ctDNA shed from tumors and present in the blood are simply too low. Heterogeneity of limited ctDNA populations can be an issue as well, making early detection and definitive identification of cancer types a challenge. Researchers have recently addressed these issues by developing methylome-based tests that cover the broad profile of cancer methylation markers in ctDNA.
Methylome-based tests look for ctDNA fragments that have had a methyl group added to a cytosine or adenine nucleotide base. Functioning as a regulatory process in cells, this pattern of methylation changes according to the cell’s activity and its dysfunction during cancer. Distinct methylation patterns, while complex, can provide information on the source of the ctDNA and its association with specific tumor types and stages of proliferation.
GRAIL Galleri® Multi-Cancer Early Detection Test
Investigators representing the CCGA Consortium8 recently developed and validated9 a multi-cancer early detection (MCED) test based on next generation sequencing (NGS) methylation analysis. Commercialized by the cancer diagnostics company GRAIL10 and termed Galleri®11, early signs indicate the test has the potential to transform the landscape of cancer screening and early detection.
The Galleri® test is designed around analysis of key methylation regions in ctDNA. Machine-learning analysis of training sets and validation of large sample populations strengthen and refine the performance of the diagnostic algorithm underlying the test. The test has been shown to exhibit overall high specificity (>99%) across a wide range of cancer types (>50). The sensitivity of the assay for early-stage tumor identification does, however, vary depending on the type of cancer. For instance, prostate cancer early-stage detection sensitivity can be as low as <25 percent, whereas detection sensitivity of head and neck cancer can reach over 75 percent. Test sensitivity also depends on the cancer stage. Interestingly, the test shows greater than 75 percent accuracy for predicting tumor signal origin, an attribute that extends over a wide range of cancer types and patient ages.
The benefits of the Galleri® test are many-fold. In addition to the ease of patient sample collection by a simple blood draw at a point-of-care location, the analysis can identify many cancer types, including unscreened and potentially lethal cancers. The test can reliably identify signal origin, providing critical information to help direct cancer confirmation and treatment. Taken together, increased diagnostic performance at the earliest possible stage can lead to dramatically lower rates of tumor stage shift and cancer progression. This in turn can result in significantly better outcomes with lower patient mortality.
The Galleri® test is currently being vetted in several high-profile population-wide clinical trials. The results of one such recent trial12, termed the PATHFINDER study, reported13 the Galleri® test detected cancer signal in 1.4 percent of 6,621 people aged 50 years and over who were not previously diagnosed with cancer. Follow-up examination confirmed that 38 percent of those identified did indeed have cancer. Of the 6,290 people who were cancer free, 99.1 percent received a negative test result, thus confirming the high specificity of the test against false positive results. Importantly, study results showed it took less than two months to confirm the screening diagnosis for cancer positive patients. These times to diagnostic resolution are significantly improved over standard diagnosis procedures and may prove especially critical in cancers for which no screening diagnostics currently exist.
Ongoing Research
Multi-cancer early detection blood testing using NGS methylation analysis is a very active research area with several new methods and recent publications hot off the press. One such study14 by investigators at the University of California, Los Angeles, involved the development of a novel assay aimed to overcome the challenges of detecting ctDNA in early cancers in a cost-effective way. The test leverages methylation detection of genomic elements associated with cancers. A key difference from some existing methods relates to the manner with which these features are targeted for analysis, focusing on small CpG islands rather than performing genome-wide methylation analysis. Although preliminary results show the specificity and sensitivity are high, the range of cancers may be limited, and the clinical utility of this assay requires validation in larger patient populations.
Outlook
Early cancer detection has traditionally been challenged by the lack of screening modalities and definitive diagnostics. State-of-the-art technologies are rapidly changing this landscape, providing solutions to fill the void for those cancers lacking screening methods and enhance the power of existing screening approaches. The emergence of multi-cancer early detection blood testing technologies, like those discussed above, may indeed change the paradigm of cancer screening and prevention, identifying cancer at the earliest possible stage and informing proper treatments to prevent progression and limit disease severity.
References:
Subscribe to Clinical Diagnostics Insider to view
Start a Free Trial for immediate access to this article